In Australia, the definition of recurrent miscarriage can vary depending on which guidelines are consulted. It may be defined as either two or more, or three or more pregnancy losses before 20 weeks gestation. Some definitions also specify that the losses must be consecutive. Around 1-2% of women experience recurrent miscarriage. Having one miscarriage after another is often highly distressing and traumatic. The variation in definitions can influence when investigations and treatments are recommended for those experiencing recurrent miscarriages.
At a glance
- Recurrent miscarriage refers to 2 or more, or 3 or more miscarriages.
- Around 1-2% of women experience recurrent miscarriage.
- There are a number of tests to check why you may be experiencing recurrent miscarriage.
- You can download our printable Recurrent Miscarriage Fact Sheet.
Testing for recurrent miscarriage
In Australia, testing for the cause of miscarriage isn’t common unless you’ve experienced recurrent miscarriage. It may also be offered if you have a personal or family history of a condition that may impact your pregnancy. If you would like testing done, it’s best to speak with your doctor or specialist as this will depend on your personal circumstances.
While testing tries to determine why you’re experiencing miscarriages, it’s not always possible to find out the cause. Some hospitals have specialist recurrent miscarriage clinics which can help women try and find the reasons and, if possible, start treatment. There are several conditions that your doctor or specialist will likely test for if you’ve experienced recurrent miscarriage.
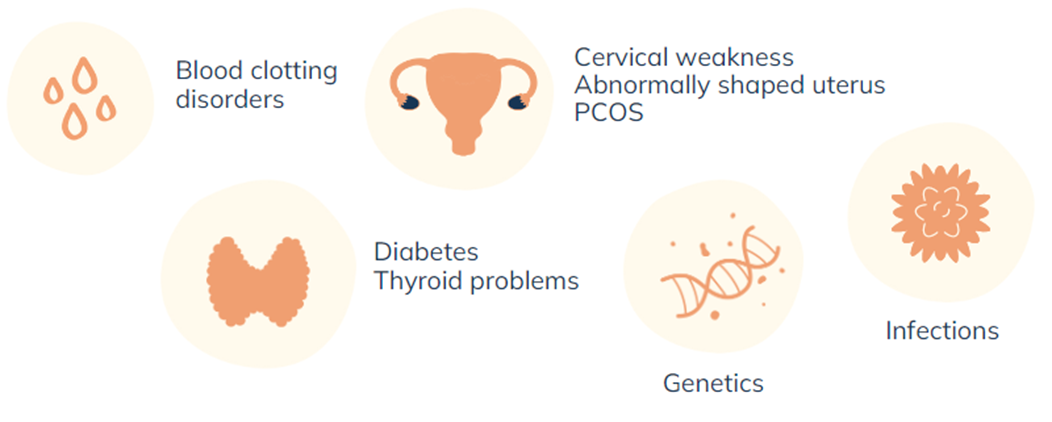
Blood clotting disorders
Antiphospholipid antibody syndrome is a blood clotting disorder. It develops when your immune system makes abnormal antibodies in the blood which then increase the risk of blood clots and pregnancy problems such as complications in placental formation and function. Research has found high levels of these antibodies in up to 15% of women who experience recurrent miscarriages.
Treatment for antiphospholipid antibody syndrome is available. If you are diagnosed with a blood clotting disorder, your specialist will go through options that may work for you.
Rhesus Negativity
If you are rhesus negative (meaning you have a minus sign following your blood type, for example, A-) and experience a miscarriage, you may be prescribed anti-D injections. This procedure prevents complications for future pregnancies if your next baby is Rhesus positive.
Genetics
Around 50-80% of miscarriages are due to chromosomal abnormalities. The vast majority are due to spontaneous chromosomal abnormalities in the parents’ sperm or egg and only a very small number to hereditary abnormalities. The older you and your partner are, the higher the risk of abnormalities.
If you have experienced recurrent miscarriage your doctor may refer you and your partner to a genetic counsellor to discuss and test for any potential genetic risks or abnormal foetal developments (heart defects, chromosomal abnormalities, spina bifida). Finding out that you have experienced miscarriage due to genetic reasons can be very distressing. A genetic counsellor can help you assess your risk of genetic disorders in future pregnancies and how you might decide about future pregnancies.
Cervical Weakness
Cervical weakness, also known as an ‘cervix insufficiency’, occurs in less than 1 in 100 women. If you have experienced late miscarriages or premature labour due to your cervix opening too early, you may have a weakened cervix. A weakened cervix can result from previous pregnancies, anatomical abnormalities that you may have been born with, particular health conditions, a history of having surgical or medical procedures involving your cervix, or a short cervix.
You may be referred for a scan to check the length of your cervix and if diagnosed, you may be advised to take progesterone or have a cervical stitch.
Abnormally Shaped Uterus
Some women have an abnormally shaped uterus. For some women this isn’t a problem but for others it can lead to problems during pregnancy or other reproductive difficulties. Having an abnormally shaped uterus can also increase the risk of miscarriage and premature birth depending on the abnormality. An ultrasound scan can be done to check whether you have an abnormally shaped uterus and if so, whether treatment such as surgery is an option.
Fibroids are common and do not usually cause any issues. However, large fibroids that impact the uterine cavity may increase your risk of miscarriage.
Uncontrolled Diabetes and Thyroid Problems
Uncontrolled diabetes and untreated thyroid problems are associated with an increased risk of miscarriage. The thyroid and having healthy levels of the hormone it makes plays a critical role in supporting pregnancy. If your thyroid levels are too high or too low it can cause pregnancy problems. Thyroid function can be checked through a blood test which measures your thyroid hormone levels and thyroid stimulating hormone in your body. In most cases, thyroid problems are relatively straightforward to treat.
Endometriosis and hyperprolactinemia can also impact your hormonal balances and your pregnancy. Endometriosis does not cause miscarriage.
What are other possible causes?
Polycystic Ovary Syndrome
There is evidence to suggest PCOS may be associated with an increased risk of miscarriage. Polycystic ovary syndrome, commonly referred to as PCOS, is a common hormonal condition affecting around 15% of women of reproductive age. Women with PCOS often have enlarged ovaries and many small cysts or follicles which fail to mature or produce eggs that can be fertilized when released from the ovaries. PCOS is one of the leading causes of infertility in women and is also associated with a range of symptoms.
If you are concerned about PCOS it’s best to see your doctor who may discuss your symptoms and medical history with you, examine you and may order some blood tests and an ultrasound to determine whether you may have PCOS.
Infections and Food Poisoning
While some infections and food poisoning can cause or increase the risk of miscarriage it is unclear what role they play in recurrent miscarriage. Infections include genital infections and sexually transmitted infections, rubella, cytomegalovirus, toxoplasmosis, listeria, salmonella and parvovirus
…once you’ve had that first miscarriage you certainly always hold that fear of something going wrong… After the first time, each subsequent pregnancy, you are on a tightrope, because you know what you’re looking for. And I know for me, I was very focused on checking for the signs, you know looking to see if it’s all going wrong
Emerging research and potential treatments
Progesterone treatment and miscarriage
There is emerging evidence from researchers at Tommy’s National Centre for Miscarriage Research that giving progesterone to women who have early pregnancy bleeding and a history of recurrent miscarriage may be beneficial and increase the chances of them having a baby. Progesterone is a hormone that is essential for maintaining a healthy pregnancy. Their research showed that women who had 3 or more previous miscarriages experienced the greatest benefit from the progesterone treatment. Importantly, the study showed that there were no safety concerns for women in taking the treatment.
Low levels of vitamin D
There is also emerging evidence from a review done by researchers at Tommy’s National Centre for Miscarriage Research that women with low levels of Vitamin D are at a significantly higher risk of miscarriage. Although a link was found, the studies were limited and further research is needed to work out whether giving vitamin D treatment before conception reduces the risk of miscarriage.
-
Why have I had a miscarriage?
Risk factors for miscarriage
-
Where can I find emotional support?
Organisations in Australia providing pregnancy loss support
-
How can I commemorate my loss?
Ways to remember your baby

The information on recurrent miscarriage has been kindly reviewed by
Professor Shaun Brennecke, AO
Head, Recurrent Miscarriage Clinic | Royal Women’s Hospital
Dunbar Hooper Professor of Obstetrics and Gynaecology| The University of Melbourne





